Canine Immune-Mediated Thrombocytopenia (ITP)
What are platelets and what do they do?
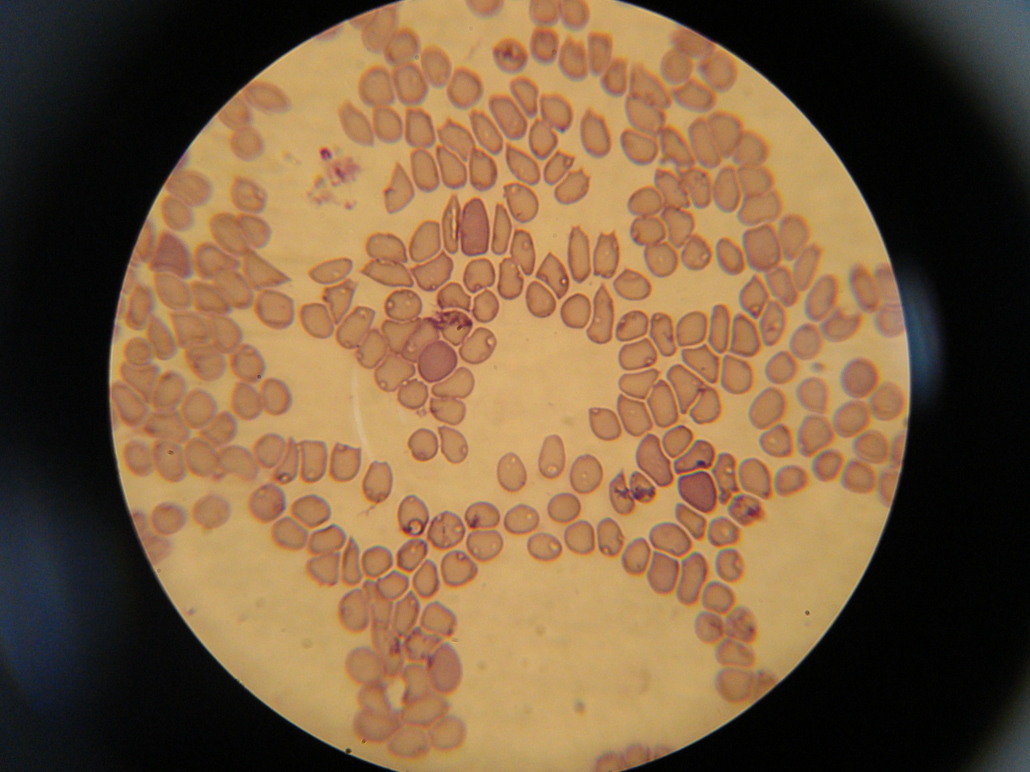
Platelets are a component of blood. Platelets are made in the bone marrow and are required to form blood clots and stop bleeding. Without them, severe bruising or bleeding can result.
- Primary haemostasis is the initial clotting that takes place after trauma to a blood vessel; this is completed by platelets
- Secondary haemostasis is the stabilization and organization of the blood clot; this is completed by coagulation proteins and is required for a clot to stay intact.
- White blood cells and Red blood cells are the other blood cells; white cells fight infection as part of the immune system; red cells carry oxygen to internal organs.
What is immune-mediated thrombocytopenia (ITP)?
ITP is a disease in which the immune system reacts against platelets just as it would against a foreign bacteria or virus. When this happens, platelets are destroyed, and bleeding or bruising often results. This often results in anaemia and leads to a number of common clinical signs. If left untreated, death can result.
- Anaemia is a low red cell count
- Thrombocytopenia is a low platelet count; it can result from a number of potential causes
- Evans’ syndrome is the combined immune mediated destruction of red blood cells and platelets
What causes ITP?
The causes of ITP are still not well understood. ITP can result from a primary immune system problem or result secondary to some other condition. Primary ITP is associated with certain breeds and is presumed to have a genetic component. Diseases that have been associated with ITP include cancerous, inflammatory, and infectious disease. Vaccines and certain drugs have also been implicated as causes of ITP. In most cases of ITP the exact cause is not identified.
- Breeds predisposed to ITP include the American Cocker Spaniel, Labrador Retriever, and Miniature Poodle.
What clinical signs does ITP cause?
ITP causes a number of clinical signs that will progress without treatment. Most of the clinical signs are associated with the bleeding that results from decreased platelet numbers. Complications, such as severe internal bleeding, can cause other more severe clinical signs.
Common signs include:
- Weakness, Tachypnea, Lethargy,
- Bruising, Oral bleeding, Epistaxis, Melena, Pale gums
Less common clinical signs include:
- Dyspnea, Sudden death
Epistaxis is nasal bleeding. Melena is a dark, tarry stool indicative of gastrointestinal bleeding. Tachypnea is increased respiratory rate. Dyspnea is breathing difficulty or significantly increased respiratory effort, Anorexia is the complete lack of appetite
What laboratory changes does ITP cause?
ITP usually causes relatively few changes on laboratory tests. Ultimately, laboratory tests are required to confirm the diagnosis of ITP and evaluate for secondary changes.
Common laboratory changes include:
- Anaemia, Thrombocytopenia,
Packed cell volume (PCV) and Haematocrit (HCT) are measures of the relative amount of red blood cells present in the blood; normal is 40% to 60%
What testing is recommended for ITP patients?
There are many goals in evaluating patients with ITP. First, the diagnosis must be confirmed and other causes of thrombocytopenia negated; secondly, other primary conditions that can cause ITP and require specific treatment must be ruled-out; and finally, prognostic and complicating factors must be evaluated.
Most patients evaluated for ITP will need the following tests:
- Complete Blood Count (CBC)
- Chemistry profile
- Urinalysis
- Coagulation testing
- Abdominal ultrasound (Abdominal ultrasound is a non-invasive test that uses sound waves to create images of internal organs and structures; this is performed along with x-rays to evaluate for underlying disease
- Chest x-rays
What complications can arise in patients with ITP?
ITP can follow both simple and complicated courses. The thrombocytopenia can cause severe bleeding that can become life threatening, especially if it can not be controlled or affects a vital organ such as the brain. Decreased oxygen delivery resulting from anaemia can cause problems with internal organ function (especially the liver and kidneys).
What treatment options are available for ITP?
ITP is a considered a treatable condition. Aggressive medical care is required, however, to help dogs with ITP and many require hospitalization. The immune response against the platelets must be controlled with immunosuppressive drugs.
Anaemia is often treated with blood transfusion therapy. Oxygen and fluid therapy are often used for supportive care during the acute presentation. Because of how complex and variable ITP is, the treatment of each patient is based on the individual presentation.
Long term treatment involves the use of immunosuppressive medications and other medications based on clinical signs. Animals are often on medications for 6-8 months after the time of presentation.
Any underlying diseases will also require treatment to help control the ITP and reduce risk of future recurrence. Drugs or vaccinations given prior to illness should be avoided as should future immune stimulation (with vaccination, for example).
Immunosuppressive medications include steroids (prednisone, dexamethasone), azathioprine, cyclosporine A, and others; these medications are often used in combination and tapered slowly over time. Transfusion therapy is provided with whole blood, concentrated red cells, or hemoglobin concentrates
What sort of long-term monitoring is recommended for ITP patients?
General recommendations for patients with ITP will depend on the individual case and what other primary or secondary conditions are identified. Generally,
CBC/platelet evaluation is performed prior to and 7-14 days after reducing immunosuppressive medications. Depending on medications used, chemistry values may be monitored periodically. Monitoring is often patient-specific and unique recommendations may be made.
What is the prognosis with ITP?
ITP carries a good prognosis in most cases, with most animals responding well to medical therapy. While anaemia itself does not usually prove fatal, the complications
of ITP can be. Gastrointestinal bleeding in particular can be difficult to control. If a dog does well during the acute disease and treatment phase, they usually do very well over the long term. While many patients can be weaned from all medications, some patients may require life-long therapy. Regardless, they usually have a excellent quality of life.